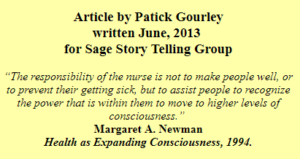
 I would have thought that after forty years in health care and thirty-five of that as an R.N. I could write on this in my sleep. That proved not to be the case.
I would have thought that after forty years in health care and thirty-five of that as an R.N. I could write on this in my sleep. That proved not to be the case.
Looking back on my own considerable number of visits to a nurse or doctor and the many thousands of interactions I have had where I was the nurse I do think the most satisfying and hopefully successful interactions were those that could be characterized as a partnership.
The realization, that I suppose was forced on me through my own HIV infection and then being in a caring capacity for many dying from AIDS, was that we, the medical establishment, were essentially helpless to make it all better. Our role seemed to be postponing and ameliorating the inevitable. This could obviously get very depressing in a hurry and I was occasionally asked over my 20 years of direct HIV care why I hadn’t “burned out”. I guess I never had a very good answer for that but looking back then and now I think I never felt that way, certainly not for very long.
Even in an AIDS clinic I was able to find joy in my work. On my best days I think it can be summed up with another quote from Newman: “The joy of nursing lies in being fully present with the clients in the disorganization and uncertainty of their lives – an unconditional acceptance of the unpredictable, paradoxical nature of life.” In other words always be aware that shit happens to everyone sooner or later. My own personal description of confronting this realty goes something like this ‘hey, we are all in this together and its always going to be messy, whether we are talking about the secret sauce from that Big Mac dripping down our chins or the drainage coming out of our private parts”.
A totally anecdotal observation on my part, and one certainly not applicable to all, is that hospice and oncology nurses tend to hang in there for a long time whereas ICU and ER folks tend to come and go much more quickly. Maybe that is why you see so many young ones in the urgent care settings and a lot more grey hair on those hanging your chemo. Perhaps this is due to a relationship in one setting predicated on a lot of adrenalin and the ‘I am here to save you” mentality while the other being more of a partnership that involves mutual problem solving around the issue for the day. Or perhaps it just takes a few decades to learn the art of compassionate communication?
I am certainly not suggesting that if you go to an ED with crushing chest pain that you should first insist on a mutual dialogue to outline a plan of care before they reach for the nitroglycerin. Give the providers all the pertinent information they ask for and then let them do their thing and hopefully they won’t have to reach for the paddles.
A key realization I came to some decades back, and I relate it to a combination of ICU nursing and the books of a physician named Larry Dossey, was that you really cannot as a provider and also as a patient view illness as bad or a failure. Margaret Newman, the nursing theorist quoted above, also planted the seeds for this in my nursing school years. I think it was Dossey who brought to my attention that health and illness are really two sides of the same coin; you cannot have the realization of one without the other.
It is, I think, when either or both the provider and the patient, perhaps even just subliminally, have the idea that someone has fucked-up that the real trouble starts. This leads to judgment and defensiveness and not an honest sharing of all the gory details that are often a part of everyone’s life. I am not implying that we don’t often make impertinent choices that have consequences, but that should not compromise the reality of the here and now and certainly does not need to define how we and our nurse or doctor will address the problem on the table at that moment. Those of us repetitive sinners can take some, rather sick I suppose, solace from the fact that a whole bunch of bad stuff happens even to those who are always doing it the ‘right way’.
What I think Newman was referring to as “moving to higher levels of consciousness” is realizing that we do not need to make so many impertinent choices.
As a patient if you have a truly nonjudgmental provider, not always easy to find, there is absolutely nothing you can tell them that will shock or if it does it will be only a transient reaction that is soon put into appropriate perspective. All the cards need to be on the table or an effective plan for addressing the issue at hand is often needlessly delayed. When honesty is involved many fewer mistakes get made in deciding on any intervention.
An example of this I heard once was “I think I got this hepatitis from a bad lime in my drink at the Triangle”, when much more helpful information would have been “do you think maybe I got this from licking butt at the bathes a couple weeks ago”. I have countless examples of this sort of magical thinking handed to me perhaps in an attempt to either not shock me or make me not think less of the person. Happily over the years of building trust with many of my clients we were able to dispense with the bullshit and cut to the chase, almost always facilitating a better outcome.
If we as both patients and providers could approach each encounter as an endeavor at caring for the soul everyone would be much better off. I’d close with another quote this one from Thomas Moore and his 1992 book Care of the Soul:
“Care of the soul…. isn’t about curing, fixing, changing, adjusting or making healthy…It doesn’t look to the future for an ideal, trouble free existence. Rather, it remains patiently in the present, close to life as it presents itself day by day…”
Gourley 6/23/2013.
